Mpox: The Rebranding Saga of a Virus
- TCWT

- Aug 28, 2024
- 8 min read
Welcome to another episode of “2024: The Year of Rebranding,” where even viruses get a makeover. The virus formerly known as "monkeypox" has gone through a name change, and now it’s “mpox”—shorter, snappier, and allegedly less offensive. But why all the fuss over a name change? Let’s dive into the twisted tale of public health, social sensitivity, and a little bit of PR wizardry.

From “Monkeypox” to “Mpox”: What’s in a Name?
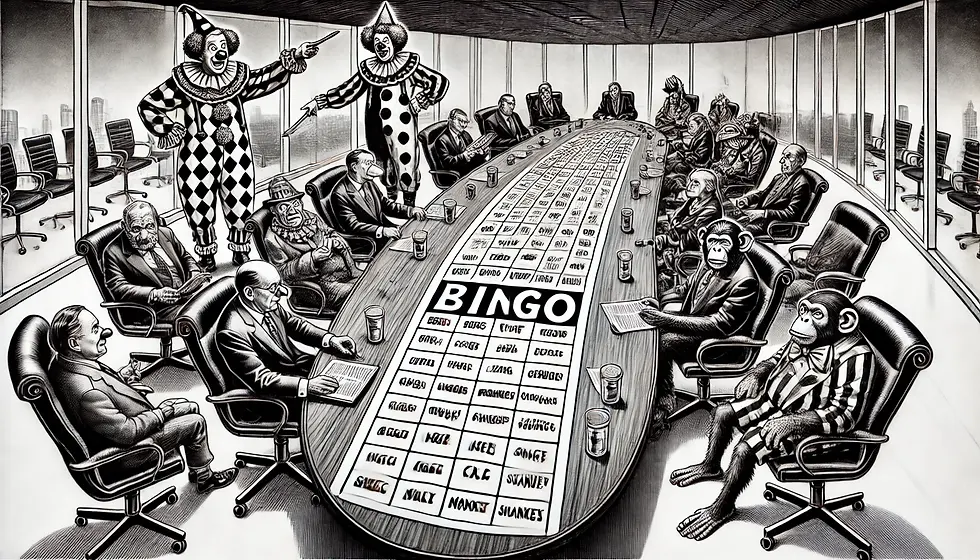
Once upon a time, in the slightly less politically correct world of virology, "monkeypox" seemed like a straightforward name. The virus was first identified in monkeys—makes sense, right? Well, not quite. You see, in the grand circus of global health, names are more than just labels; they’re a delicate dance between science, sensitivity, and spin control.
The World Health Organization (WHO) decided it was time to drop the “monkey” from monkeypox. Why? To avoid stigmatization and prevent any unintended racist undertones. Apparently, the word "monkey" can conjure up all sorts of problematic imagery—especially given the virus’s historical links to Africa. The fear? That people might make unsavory, subconscious associations between the virus and people of African descent. Because nothing says inclusivity like assuming everyone is a closet racist just waiting to connect dots between a primate and a continent.
Learn more about the WHO’s rationale for the name change here.
The Logic Behind the Name Change: Avoiding a PR Disaster
Let’s get one thing straight: public health is as much about optics as it is about medicine. The WHO, ever the maestro of this balancing act, wanted to avoid any whiff of controversy. Naming a disease after an animal linked to a specific region? That’s a PR nightmare in the making. Instead, they opted for “mpox”—a sleek, non-threatening rebrand. No animals, no regions, no fuss.
Think of it as a linguistic facelift. "Mpox" is the new, neutral label that promises not to offend anyone or evoke any unintended connotations. It’s like calling a nuclear meltdown a “thermal event”—sure, it doesn’t change the severity, but it sounds a lot nicer on the news.
Wait, Wasn’t There a 2022 Outbreak? Why Did That News Disappear?
Ah, the 2022 mpox outbreak—a brief but intense media frenzy that suddenly went silent faster than you could say “COVID fatigue.” So, what happened? Why did the headlines about mpox vanish quicker than your New Year’s resolutions?
Well, it turns out the initial surge of panic was met with an equally aggressive public health response. Countries rolled out contact tracing, isolation protocols, and even some vaccination efforts using smallpox vaccines. And guess what? The numbers started to drop. A crisis averted, or so it seemed.
But there’s more to the story. As case numbers fell, so did the media’s interest. The world had other pressing issues—war in Ukraine, economic woes, and oh yeah, that lingering little thing called the COVID-19 pandemic. It’s hard for a new virus to keep the limelight when it’s competing against a global pandemic and geopolitical crises. Plus, there was the added complexity of public fatigue. After two years of COVID-19, the world was tired of hearing about the next great health scare. Unless mpox could somehow reinvent itself as the next great Netflix thriller, it wasn’t going to hold people’s attention for long.
For a detailed timeline of the 2022 mpox outbreak and response measures, check out this report here.
Stigma and Sensitivity: Walking the Public Health Tightrope
Another reason for the quiet fade-out of mpox news might have been the demographic most affected: men who have sex with men (MSM). The virus was particularly prevalent in this community during the 2022 outbreak, sparking concerns about how to communicate risk without stigmatizing an already marginalized group. Public health officials faced a delicate balancing act: raise awareness without fueling discrimination. And let’s not forget, it wasn’t just MSM communities; there were also rare cases involving children, adding another layer of complexity to the narrative.
Did the WHO and other health organizations want to avoid a repeat of the early days of the HIV/AIDS epidemic when misinformation and stigma ran rampant? Maybe. We believe they wanted to make sure the public knew that anyone could contract mpox, regardless of their sexual orientation. But in doing so, they may have toned down the messaging a bit too much, contributing to the perception that the virus was “silenced” in the media.
Is Mpox Still a Thing in 2024?
Fast forward to 2024, and guess what? Mpox is still spreading. Yep, despite the name change, the virus didn’t just pack up and leave. In fact, the WHO recently declared mpox a public health emergency of international concern. A new, more transmissible strain has emerged, primarily affecting several African countries, including the Democratic Republic of the Congo, Burundi, Kenya, Rwanda, and Uganda. Over 14,000 cases and 524 deaths have been reported this year alone—a significant increase from previous years.
Read the latest updates on the current mpox outbreak here.
Mpox spreads through close contact with infected individuals or contaminated surfaces, proving once again that while you might be able to change the name, you can’t change the nature of a virus. And as for public health efforts, it’s all hands on deck. The WHO is deploying vaccines and ramping up surveillance to try and contain this pesky pathogen.
The Verdict: What’s in a Name? A Whole Lot of PR
So, what have we learned from the great mpox rebrand of 2024? Names matter, but maybe not for the reasons you’d think. For health organizations, choosing the right name is a high-stakes game that involves more than just science—it’s about managing perceptions, avoiding stigma, and, let’s face it, a bit of damage control.
Was it the right move to rename monkeypox to mpox? Depends on who you ask. Some see it as a necessary step to foster a more inclusive and sensitive global health environment. Others see it as a classic case of over-correction, fixing a problem that might not have existed in the first place. In any case, one thing’s for sure: in the world of public health, even the names are contagious.
How to Avoid Mpox: Practical Steps for Prevention

While the renaming saga of "monkeypox" to "mpox" might have grabbed headlines, it’s essential to remember that mpox is still a contagious disease with real health implications. So, how do you protect yourself and others from catching it? Here’s a comprehensive guide to minimizing your risk of infection:
1. Understand the Transmission Routes
Mpox primarily spreads through close, prolonged contact with an infected individual. This can include:
Direct skin-to-skin contact with lesions, rashes, or body fluids of an infected person.
Respiratory droplets during prolonged face-to-face contact, particularly in enclosed spaces.
Contact with contaminated objects like clothing, bedding, towels, or surfaces that have come into contact with an infected person.
Understanding these transmission routes helps you identify situations where the risk of exposure might be higher, such as crowded events, close physical contact settings, or shared living spaces.
2. Practice Good Hygiene
Maintaining personal hygiene is crucial in reducing the spread of mpox:
Wash your hands regularly with soap and water for at least 20 seconds, especially after touching surfaces in public places, using the restroom, or before eating.
Use alcohol-based hand sanitizer (with at least 60% alcohol) when soap and water are not available.
Avoid touching your face, eyes, nose, and mouth with unwashed hands.
3. Avoid Close Contact with Infected Individuals
If someone you know has mpox or is displaying symptoms (such as a rash, fever, or swollen lymph nodes):
Maintain a safe distance and avoid physical contact.
Refrain from sharing personal items like utensils, bedding, towels, or clothing.
Isolate the infected individual in a separate room, if possible, and limit their contact with others in the household.
4. Wear Protective Gear When Necessary
If you are in a high-risk setting (like healthcare facilities or if you are caring for someone with mpox at home):
Wear a face mask to protect against respiratory droplets, especially in enclosed or crowded spaces.
Use gloves when handling potentially contaminated materials, such as bedding or clothing of an infected person.
Consider using gowns or protective clothing when caring for someone with mpox or when in direct contact with an infected person.
5. Disinfect and Clean Frequently
Ensure that you regularly clean and disinfect commonly touched surfaces and items:
Use household disinfectants effective against the virus to clean surfaces like countertops, doorknobs, and bathroom fixtures.
Launder clothing, bedding, and towels in hot water and dry them on high heat to kill any potential virus particles.
Avoid shaking out laundry from an infected person, as this can disperse the virus into the air.
6. Stay Informed and Follow Public Health Guidance
Keeping up with the latest guidelines from reputable health organizations is key:
Follow the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) for updated guidelines on mpox.
Get vaccinated if eligible and if a vaccine is available in your area, especially if you are in a high-risk category or live in an outbreak region.
Monitor local health advisories to stay informed about the status of mpox in your community and any additional measures that might be recommended.
7. Address Stigma and Misinformation
Remember, misinformation and stigma can hinder effective disease prevention and control:
Educate yourself and others about the facts of mpox transmission and prevention to avoid spreading fear or stigma.
Support open and non-judgmental communication about mpox to ensure people feel comfortable seeking medical help and following public health advice.
By following these practical steps, you can help prevent the spread of mpox and protect yourself and your community from this infectious disease. Stay vigilant, stay informed, and continue to prioritize your health and safety.
Conclusions: Navigating the Mpox Landscape
The story of mpox, from its rebranding saga to its ongoing spread, offers a fascinating glimpse into the complexities of modern public health communication. It underscores the delicate balance between scientific accuracy, social sensitivity, and effective disease control. As we navigate this evolving landscape, several key takeaways emerge:
Language Matters in Public Health:
The renaming of "monkeypox" to "mpox" highlights the power of words in shaping public perception and avoiding unintended stigma. While some may see the change as an over-correction, it reflects a broader commitment to inclusive and non-discriminatory public health practices.
Public Attention is Fleeting:
The initial media frenzy around the 2022 mpox outbreak illustrates how quickly public focus can shift. Despite the initial panic, the disease seemingly "disappeared" from the headlines as cases declined and other global crises took center stage. This reminds us of the importance of sustained awareness and preparedness, even when a health threat seems under control.
Stigma and Sensitivity Are Crucial:
The approach to communicating about mpox has been shaped by lessons learned from past public health challenges, such as the HIV/AIDS epidemic. Avoiding stigmatization and ensuring that at-risk communities receive targeted, supportive communication is vital in any outbreak response.
Mpox Remains a Public Health Concern:
Despite the name change and reduced media coverage, mpox is still very much a public health concern in 2024, especially with the emergence of a new, more transmissible strain. Continued vigilance, effective public health measures, and global cooperation are essential in managing the disease's spread.
Prevention is Key:
Understanding how mpox spreads and taking practical steps to prevent infection are crucial. Public health efforts need to focus on education, vaccination, and community support to ensure comprehensive and effective disease prevention.
The Future of Public Health Communication:
The mpox case also raises questions about the future of public health messaging in a hyper-connected, globalized world. As health organizations strive to balance transparency, sensitivity, and clarity, the lessons learned from mpox will likely inform future strategies for addressing emerging health threats.
In conclusion, while the renaming of mpox may seem like a small detail in the grand scheme of global health, it serves as a potent reminder of the complexities involved in disease management. By staying informed, taking preventive measures, and fostering an inclusive public health environment, we can better navigate the challenges that diseases like mpox present. After all, in the battle against infectious diseases, knowledge—and a bit of careful communication—remains our best weapon. Let's not repeat the COVID-19 shit show please.
















Comentários